Traumatic Brain Injury
A concussion is a type of traumatic brain injury (TBI) that results from a bump, blow, or jolt to the head, or a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce or even twist inside the skull, stretching and damaging brain cells and creating chemical changes in the brain.
Falls and car crashes are the most common causes of TBI-related hospitalizations among older adults.
There are three main types of TBI:
- Mild TBI or concussion
- Moderate TBI
- Severe TBI
Most TBIs that occur in older adults are mild TBIs or concussions.
TBIs are preventable, but they remain a serious public health concern resulting in death and disability for thousands of older Americans each year. Older adults are more likely to have a hospital stay following a TBI compared to all other age groups.
Falls and motor vehicle crashes are two of the leading causes of TBI-related hospitalizations among older adults. The good news is that you can lower your chance of getting a TBI by following steps to prevent a fall or motor vehicle crash.
TBIs may be missed or misdiagnosed in older adults because symptoms of TBI overlap with other medical conditions that are common among older adults, such as dementia. Your health care provider should check you for signs and symptoms of TBI if you have fallen or were in a car crash.
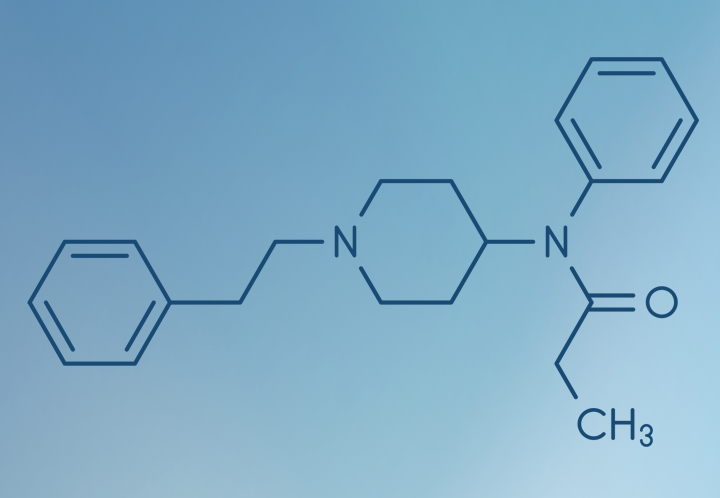
This is especially important if you are taking blood thinners, such as:
- Anticoagulants such as warfarin (Coumadin), rivaroxaban (Xarelto), and apixaban (Eliquis)
- Antiplatelet medications such as clopidogrel (Plavix), ticagrelor (Brilinta), and acetylsalicylic acid (Aspirin)
These medicines may increase the risk for bleeding in the brain following a TBI. Bleeding in the brain after a TBI may put a person at risk for more severe injury or death.
Physical
- Bothered by light or noise
- Dizziness or balance problems
- Feeling tired, no energy
- Headaches
- Nausea or vomiting (early on)
- Vision problems
Thinking and remembering
- Attention or concentration problems
- Feeling slowed down
- Foggy or groggy
- Problems with short- or long-term memory
- Trouble thinking clearly
Social or emotional
- Anxiety or nervousness
- Irritability or easily angered
- Feeling more emotional
- Sadness
Sleep
- Sleeping less than usual
- Sleeping more than usual
- Trouble falling asleep
Thinking and learning
- Difficulty understanding and thinking clearly
- Trouble communicating and learning skills
- Problems concentrating
- Difficulty remembering information
Motor skills, hearing, and vision
- Weakness in arms and legs
- Problems with coordination and balance
- Problems with hearing and vision
- Changes in sensory perception, such as touch
Emotion/mood
- Feeling more emotional than usual
- Nervousness or anxiety
- Feeling more angry or aggressive than usual
- Sadness, depression
Behavior
- Trouble controlling behavior
- Personality changes
- More impulsive than usual
You should see your health care provider if you get a TBI or concussion. Your health care provider may have treatment to help speed up your recovery.
- Most people with a mild TBI or concussion can recover safely at home following a medical check-up. You may experience short-term symptoms and feel better within a couple of weeks or months.
- People with a moderate or severe TBI may need ongoing care to help with their recovery. You may have long-term or lifelong effects from the injury.
If you do get injured, it's important to know how to spot a concussion or TBI and what to do if you think you have one.
Recovering from a concussion or other TBI is different for each person.
- Recovery depends on many things such as:
- Your health before the injury
- Type and severity of your TBI (mild, moderate, or severe)
- Access to health care and specialized TBI care
- Family and other social support
- It's important to get plenty of rest after the injury when symptoms are most severe to help your brain heal.
- Ask your health care provider questions about your recovery:
- When can I get back to normal activities?
- Is there any activity I should not do, such as exercise?
- When can I return to driving (if you currently drive a car)?
- What medicines should I take (or stop taking)?
- Can I take any other medicines, for example, acetaminophen (Tylenol)?
- What other problems, if any, should I look for related to this injury?
- Will I need any special treatment or therapy, like physical therapy?
- When do you want to see me next?
Contact Information
Mailing Address:
Oklahoma State Department of Health
Injury Prevention Service
123 Robert S. Kerr Ave., Suite 1702
Oklahoma City, OK 73102-6406
Physical Address:
Oklahoma State Department of Health
Injury Prevention Service
123 Robert S. Kerr Ave.
Oklahoma City, OK
Telephone: (405) 426-8440
Fax: (405) 900-7588
Email: injury@health.ok.gov